Exocrine pancreatic insufficiency IBS
IBS patients presenting with limited exocrine pancreatic output. Usually with concommitant diabetes or other metabolic disorder

Number of cases
Mean age
Rate of success
Treatment duration
Most common symptom
Most common culprit
The digestion of animal derived food relies vastly on the adequate excretion of pancreatic enzymes. Food particles that reach our small intestine, after proper preparation in our stomach, are being eluted by pancreatic and liver products which consist, mainly, of bicarbonates, bile and enzymes. These enzymes, which belong to the protease, lipase and amylase classes, are responsible for the complete degradation of peptides, lipids and sugars, respectively. If these enzymes are not sufficient, undigested particles will be forwarded downstream and an array of unwanted side effects will take place, like bloating, diarrhea, dysbiosis etc.
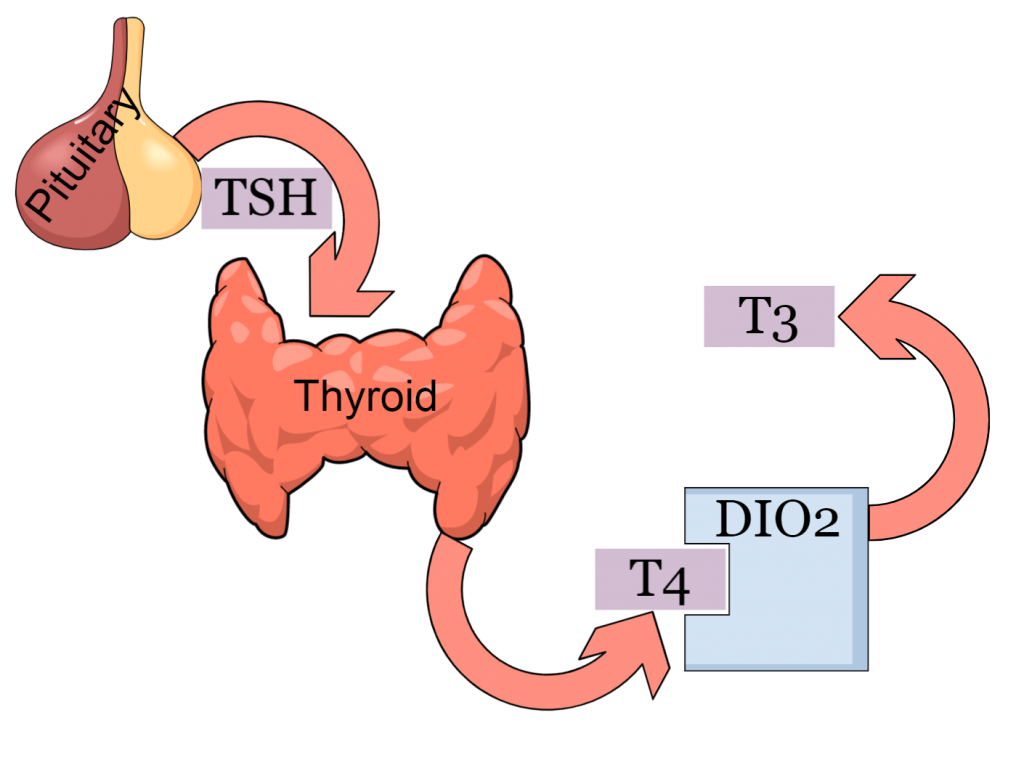
Most commonly, but not necessarily, exocrine pancreatic insufficiency (EPI) will appear within the context of other diseases, like diabetes, chronic pancreatitis, bile obstruction, celiac disease or after several surgeries, like gastric dissection and colectomy. Due to the fact that exocrine pancreatic insufficiency is thought to be a rare clinical entity, it is commonly being overlooked. The main problem here is that in many cases, EPI is the central root of gut problems labeled as irritable bowel syndrome. Another problem is that most physicians, and patients, think that abdominal ultrasounds or CT scans can exclude any pancreatic role in their disease; this is not true. Imaging techniques may only find tissue alterations, but they cannot, in any way, measure the enzymatic output of the organ. This is why it should be ordered every time symptoms like diarrhea, early satiety or floating stool with rapid transit time are reported by the patient.
Leeds, John S., et al. “Some patients with irritable bowel syndrome may have exocrine pancreatic insufficiency.” Clinical Gastroenterology and Hepatology 8.5 (2010): 433-438.
Olmos, Juan I., et al. “Exocrine Pancreatic Insufficiency is Undiagnosed in Some Patients with Diarrhea-Predominant Irritable Bowel Syndrome Using the Rome IV Criteria.” Digestive Diseases and Sciences (2022): 1-10.
Olmos, Juan I., et al. “Exocrine Pancreatic Insufficiency is Undiagnosed in Some Patients with Diarrhea-Predominant Irritable Bowel Syndrome Using the Rome IV Criteria.” Digestive Diseases and Sciences (2022): 1-10.
Michael is now a 56 years old bus driver. He has been working for the past 15 years driving at the line which connects the port of Piraeus to the national airport of Athens. This means that all these years he’s been on a shift working schedule including weekly cycles of night shifting. By age 49, he was diagnosed with type II diabetes. Despite his efforts to control his blood sugar with diet and exercise, a year later he started insulin therapy. When diarrhea and bloating begun he did not correlate it with his diabetes diagnosis. Neither the 6 different physicians he visited. He was one of the many diabetic patients who told me the phrase “But I have already checked my pancreas and it all seem to be fine”.
The timing of our social activities (work, exercise, meals, socializing etc) has a direct and profound effect on pancreatic function
Both the pathology of diabetes and insulin treatment confer a great impact on the development and the maintenance of the gut microbiome
The ongoing loss of nutrients due to malabsortpion creates a vicious cycle bewteen exocrine insufficiency and IBS symptoms
Michael had at least one obvious cause of EPI; and that is diabetes. But in addition he also had several other less important possible causes that altogether may explain the complete array of his symptoms. My guess was that all three symptoms that Michael reported as major (i.e. diarrhea and urgent defecations, bloating and abdominal pain) are all secondary manifestations to EPI. EPI makes a whole bunch of food particles to rot or being fermented abnormally in the patient’s colon, leading to a very inconsistent and maldistributed production of air and to a constant secretion of water and mucus form the intestinal walls.
Stool consistency is highly influenced by the proportions of nutrients (fat-soluble vs water-soluble) reaching the colon and the excreting capacity of the colon at that specific time
Exocrine pancreatic insufficiency and the resulting enzyme inadequacy leads to defective food degradation. Indigested food particles may cause both stomach and bowel cramps
The bacterial fermentation of unabsorbed food is much more prominent in patients suffering from exocrine pancreatic insufficiency
While early satiety is mostly evident in people suffering from diabetic gastroparesis, it may also appear in the context of exocrine pancreatic insufficiency
Michael’s pancreatic elastase was close to zero. This resulted in diarrhea but also in the difficulty in regulating diabetes. In addition, Akkermansia a characteristic bacterium, which has been associated with proper glucose regulation, was absent. The rest of the findings related to large eradication of probiotic cultures, recovery of high fat concentration on stool (steatorrhea) and recovery of several fungi, such as Geotrichum, which possesses a well-defined lipase activity.

Akkermansia muciniphila deficiency
Akkermansia, besides being a commensal bacterium, it is now considered an glucose homeostatic gut mechanism. In fact it seems that metformin works only when Akkermansia is present

Exocrine pancreatic insufficiency
Diminished pancreatic output may explain all the patient’s symptoms, including malabsorption, urgency, diarrhea and even glucose fluctuations

Steatorrhea
Malabsorption of fat molecules may explain the fatigue, weight loss and floating droplets of oil on the toilet water
Probiotic sterility
Probiotic sterility leads to abnormal fermentation of starch, sugars and fiber. Bloating and gas are main symptoms
The plan I prepared for Michael had two main targets: Exocrine pancreatic insufficiency and dysbiosis. Enzyme supplementation is never sufficient for full symptom remission, and only after the repopulation of beneficial bacteria the social life of the patient is restored. Of course, animal enzymes are not enough, since Michael’s microflora depletion will not allow him to digest neither plant derived fiber nor complex carbohydrates. IBS treatment in diabeteic patients always has an additional metabolic part.

I saw Michael 6 weeks later. His blood glucose levels were stabilized, his stools were regular and he was feeling great. There were only minor disturbances in his stool consistency and some bloating during this period but in general he was feeling 80% better. I told him that these incidents will gradually disappear and that maybe the die-off effect was to blame. I advised him to stay on a strict 15:9 intermittent fasting schedule and to stay away from alcohol. Our last communication took place 6 months later. He was very stable and he had reduced his daily insulin shot to 16 units from 24 units before his therapy.
IBS patients that present with EPI are usually chronically undiagnosed. The main reason is that their symptoms are easily categorized as “normal complications of their primary disorder” and thus left untreated. The most common phrase I hear is that they have been told “if we take care of your diabetes, your gut symptoms will disappear”. However, this is not true – unless the lipid absorption gets restored, blood glucose fluctuations become more often and more intense. EPI patients must be well informed that full pancreatic restoration is not possible. Several times I have seen a small to medium restoration but generally not to a significant level. They must be taught how to plan their meals, and they should always have in mind that they should not leave their digestive function uncontrolled. First, EPI symptoms will appear, next their microflora will deteriorate and finally malnutrition and glucose imbalances will begin.
- EPI may manifest in the context of autoimmune disorders, like psoriasis, celiac disease and spondyloarthropathies and after several operations, like cholecystectomy, gastrectomy and colectomy
- Diarrhea bloating and early satiety are the most prominent symptoms, whereas other symptoms like multiple defecations and weight loss are common
- Diabetes and several other metabolic disorders are linked to inferior pancreatic function and lead to exocrine pancreatic insufficiency (EPI), even in the absence of diabetes
- The gut is interconnected both directly and indirectly with almost all other organs and thus a multidisciplinary approach is often required
- Lifestyle choices play a determining role in the complete remission. Most important are regular fasting periods, respect of inner clock processes (sleep, training) and a gut nourishing diet