Breastmilk and microbes: Breastfeeding is much more than …. feeding
Breastfeeding shapes the infant microbiome as it contains live beneficial bacteria that support the development of a healthy microbial community

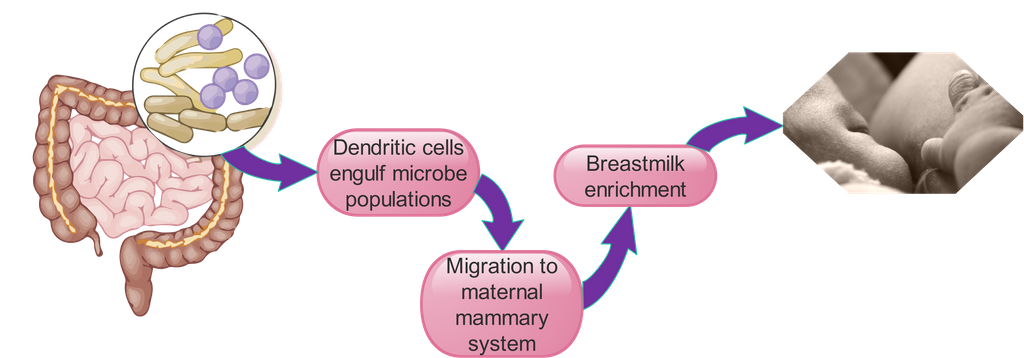
Breastfeeding is a dynamic process that helps to shape the infant gut microbiome, the community of bacteria, viruses, fungi, and other gut microorganisms. Breast milk, which is rich in beneficial bacteria and prebiotics, plays a crucial role in establishing and shaping the early life gut microbiome. The dynamic nature of breastfeeding, including the introduction of new bacterial populations and the enrichment of the milk with beneficial bacteria from the maternal gut, helps to ensure that the infant receives the right balance of nutrients and beneficial bacteria to support the development of a healthy microbial community
Breastfeeding is a dynamic process
Breast milk is more than just a source of nutrition for infants – it also plays a crucial role in shaping the development of the infant microbiome. Human milk oligosaccharides (HMOs), a type of carbohydrate found in breast milk, have been shown to alter developmental trajectories by influencing the composition and function of the intestinal microbiota during the first year of life. HMOs are not digested by the infant, but are fermented by gut bacteria, leading to the production of short-chain fatty acids that have a variety of health benefits. By supporting the growth of beneficial bacteria and inhibiting the growth of harmful bacteria, HMOs promote a healthy microbial community in the infant gut. This, in turn, has a positive impact on the overall health and development of the infant.
From early life gut maturation...
Digestion
The microbiome plays a crucial role in the digestion of food and the absorption of nutrients. It helps to break down complex sugars and fibers that the body cannot digest on its own and also produces certain vitamins, such as vitamin K and B-vitamins.
Immunity
The microbiome helps to protect the body against illness and infection by producing antimicrobial substances and stimulating the immune system. It also helps to prevent the overgrowth of harmful bacteria and other microorganisms.
Metabolism
The microbiome plays a role in metabolism by influencing the production and breakdown of certain hormones and chemicals in the body. It has also been linked to the development of obesity and other metabolic disorders.
Mental health
The microbiome has been found to play a role in mental health and has been linked to conditions such as depression, anxiety, and autism.
Allergies and asthma
A healthy microbiome has been shown to reduce the risk of developing allergies and asthma.
Skin health
The microbiome has a role in maintaining the health of the skin by protecting against infections and influencing the production of oils and other substances that keep the skin hydrated and healthy.
Postbiotics
Postbiotics are metabolic byproducts produced by the microbiome that have various health benefits. For example, certain postbiotics have been found to have anti-inflammatory effects and have been linked to the prevention of certain diseases.
Neonatal development
The microbiome plays a crucial role in the development of newborns, especially in the first few months of life. A healthy microbiome can help to support growth and development and reduce the risk of certain health issues.
Breast milk shapes the infant microbiome
Breast milk also contains prebiotics
Lactose: Lactose is a disaccharide that is broken down by lactase, an enzyme present in the small intestine, into its component monosaccharides, glucose and galactose. These monosaccharides can then be absorbed and used for energy.
Lacto-N-biose (Gal-1-3GlcNAc): Lacto-N-biose is a structural component of some HMOs .
N-acetyllactosamine (Gal-1-4GlcNAc): Like lacto-N-biose, N-acetyllactosamine is a structural component of some HMOs
Fucose: Fucose is a monosaccharide that can be linked to other sugars to form fucosylated HMOs. It plays a role in the immune system by serving as a ligand for certain receptors on immune cells.
Sialic acid: Sialic acid is a monosaccharide derivative that can be linked to other sugars to form sialylated HMOs. It plays a role in the immune system by serving as a ligand for certain receptors on immune cells.
20-fucosyllactose (20-FL): 20-FL is an HMO that is fucosylated at the terminal position. It serves as a ligand for certain receptors on immune cells.
Lactodifucopentaose: Lactodifucopentaose is an HMO that is fucosylated at the terminal position.
Lacto-N-tetraose: Lacto-N-tetraose is an HMO that contains N-acetylglucosamine at the terminal position.
20-sialyllactose: 20-sialyllactose is an HMO that is sialylated at the terminal position.
What factors influence gut microbiota shaping
The infant microbiome begins to develop in utero, but it is largely influenced by the environment after birth. This means that the types of bacteria and other microorganisms present in the infant microbiome are influenced by various factors such as diet, environment, mode of delivery, and other exposures.
Gestation
During pregnancy, the developing fetus is exposed to bacteria and other microorganisms from the mother's microbiome, which can influence the development of the infant microbiome.
Breastfeeding
Breast milk contains a range of beneficial bacteria and prebiotics that can help to support the development of a healthy microbiome in infants. Formula-fed infants may have a different microbiome than breastfed infants, as formula does not contain the same types of bacteria and prebiotics found in breast milk.
Solids introduction
The age at which solids are introduced can also influence the infant microbiome. Introducing solids earlier or later than recommended may alter the types of bacteria present in the infant microbiome.
Mode of delivery
The infant microbiome is largely shaped by the environment after birth. For example, infants who are born via cesarean section may have a different microbiome than infants born vaginally, as they are exposed to different types of bacteria during delivery.
Antibiotics
Antibiotic treatments can also alter the microbiome, as they can kill both harmful and beneficial bacteria
Geographic location
Geographic location can also play a role in shaping the infant microbiome, as different regions of the world have different bacterial exposures and exposures to different types of bacteria can affect the infant microbiome.
Children update milk composition through saliva
Mothers ship microbes from their gut to the breast
Milk has different composition between two feedings
Tips for keeping the milk nutritious
Eat a diverse and healthy diet
A healthy and varied diet can help to support the production of breast milk and may increase the levels of probiotics and prebiotics in breast milk. Aim to include a variety of whole, unprocessed foods in your diet, including fruits, vegetables, whole grains, and lean proteins
Include seasonal vegetables
Seasonal vegetables are fresher and more nutrient-dense than out-of-season produce, and they may contain a wider range of beneficial nutrients and phytochemicals
Avoid processed foods
Processed foods are often high in additives, preservatives, and other artificial ingredients. Limiting your intake of processed foods and focusing on whole, unprocessed foods may help to improve the quality of breast milk
Exercise regularly
Regular physical activity can help to improve overall health and wellness, and has positive effects on breast milk production and quality
Take probiotics
Taking probiotics may help to increase the levels of beneficial bacteria in the gut, which may be reflected in the breast milk
Eat prebiotic-rich foods
Prebiotics are compounds that serve as a food source for beneficial bacteria. Including prebiotic-rich foods in your diet, such as onions, garlic, asparagus, and leeks, may help to increase the levels of prebiotics in breast milk
Stay hydrated
Drinking plenty of water and other fluids can help to support the production of breast milk and may help to improve its quality
Avoid pesticides
Pesticides, such as glyphosate, can be harmful to both human health and the environment. Limiting your exposure to pesticides, such as by choosing organic produce or growing your own fruits and vegetables, may help to reduce the levels of pesticides in breast milk
Avoid heavy metals
Heavy metals, such as lead and mercury, can be harmful to health and may be present in certain foods and the environment. Limiting your exposure to heavy metals, such as by avoiding certain types of fish or not smoking, may help to reduce the levels of heavy metals in breast milk
Choose healthy fats
Healthy fats, such as olive oil, avocado, and nuts, are an important part of a healthy diet and support the production and quality of breast milk