Aller – G -Section
Mode of delivery and allergies
The connection and what to do about it

No question that delivery via c-section has saved million of lives, many centuries now. It is a very safe, rarely complicated procedure which ensures that every possible factor that may endanger the fetus, or the mother is eliminated. Up until minutes before birth, a c-section newborn has been exposed to the exact same things a naturally born one has. But the moment the baby is separated, a very big difference appears. A difference capable of defining the likelihood of the baby presenting with several immune dysregulations later in life. The microbiome colonization potential.
Factor or co-factor?
Not one, nor two. Over 25 studies have linked mode of delivery with the likelihood of the newborn to present with an atopic disease sometime later in his life. The exact time when symptoms appear is not the same to all of them, as it depends on other factors, like exposure to animals or to environmental pollution, diet, length of breastfeeding and others. Nevertheless, their gut immune system is already primed to present more easily with atopic symptoms.
When do we become hosts?
As soon as a child is born, some colonies of microbes already exist in the intestine and lungs. These populations come from 3 key sources: the maternal urogenital system, the mother’s mouth and her gut. But the main batch of microbes that will thrive and define the newborn’s flora for the next few years is the one that the child acquires during the passage from the mother’s vagina. The newborn’s lips and tongue are the main carriers of this bacterial transfer and this is the main reason why mother’s vagina must not be infected during or right before labor.
How is beneficial flora defined?
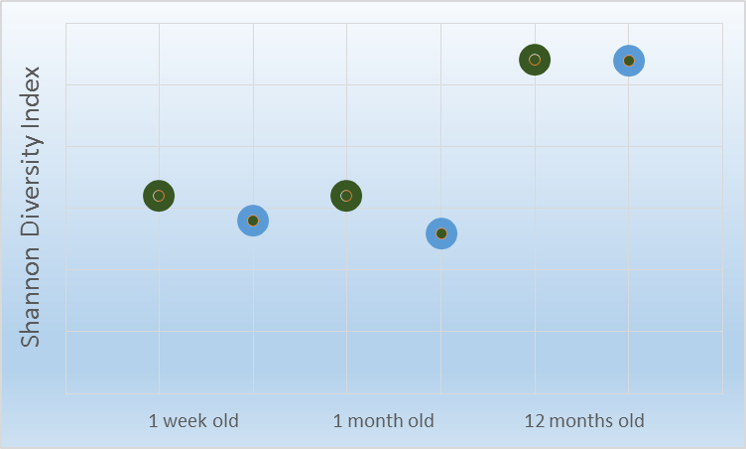
An objective way of measuring the health of a bacterial ecology is its diversity. It is accepted that the greatest the diversity of a specific microbial ecology the better it serves its own purposes, as well as the host’s homeostasis. One of the indices that’s used to measure diversity is called the Shannon Diversity Index (SDI). Using SDI, a Swedish team, back in 2013 (1) studied 47 boys, aged 7, whose stool had been collected and assessed three times during their first year of life (1 week, 1 month and 1 year old). They concluded that children who presented with asthma (blue circles) had a much lower SDI when measured at 1 week and 1 month but not at 1 year after birth, in comparison with healthy children (green cycles). This means that microbiome composition during these early months is crucial for the development of asthma even years later.
Histamine is a major contributor to atopy
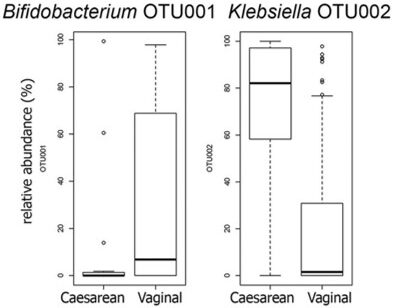
Another reason asthma and atopic diseases are more prevalent in children born via s-section is histamine. Histamine is a well known mediator of itching, wheezing and part of all atopic diseases’ mechanism. This is why part of the pharmaceutical treatment consists of anti-histamines. What if cesarean born children had more histamine entering their bloodstream at all times? In fact this is true, since a big part of the total histamine load comes from bacterial processes. Bacteria that reside in the gut lumen. These bacteria use histidine, a natural amino acid derived from food and produce histamine. Until a threshold this is fine. If the populations that produce histamine, though, are overgrown, the total histamine burden that’s produced will grow exponentially and predispose for allergic diseases. Such a bacterium is Klebsiella. Several strains of Klebsiella are potent histamine producers. A 2015 study, published in mBio, the journal published by the American Society of Microbiology (2) found that children born via c-section have enormous amounts of Klebsiella on their stool and very low amounts of a beneficial strain of Bifidobacterium. This means that right from birth, children born with cesarean produce larger amounts of histamine.
So what can be done now?
What can’t be done for sure is give birth to your child again. But there are many things that may help restore the baby’s intestinal ecology. The most important action you should take is simply breastfeeding. Breastmilk, besides the valuable nutrients, cellular building blocks and calories it contains, it is a source of constant microbe replenishment, right form mother’s gut.